What Is Diabetes?
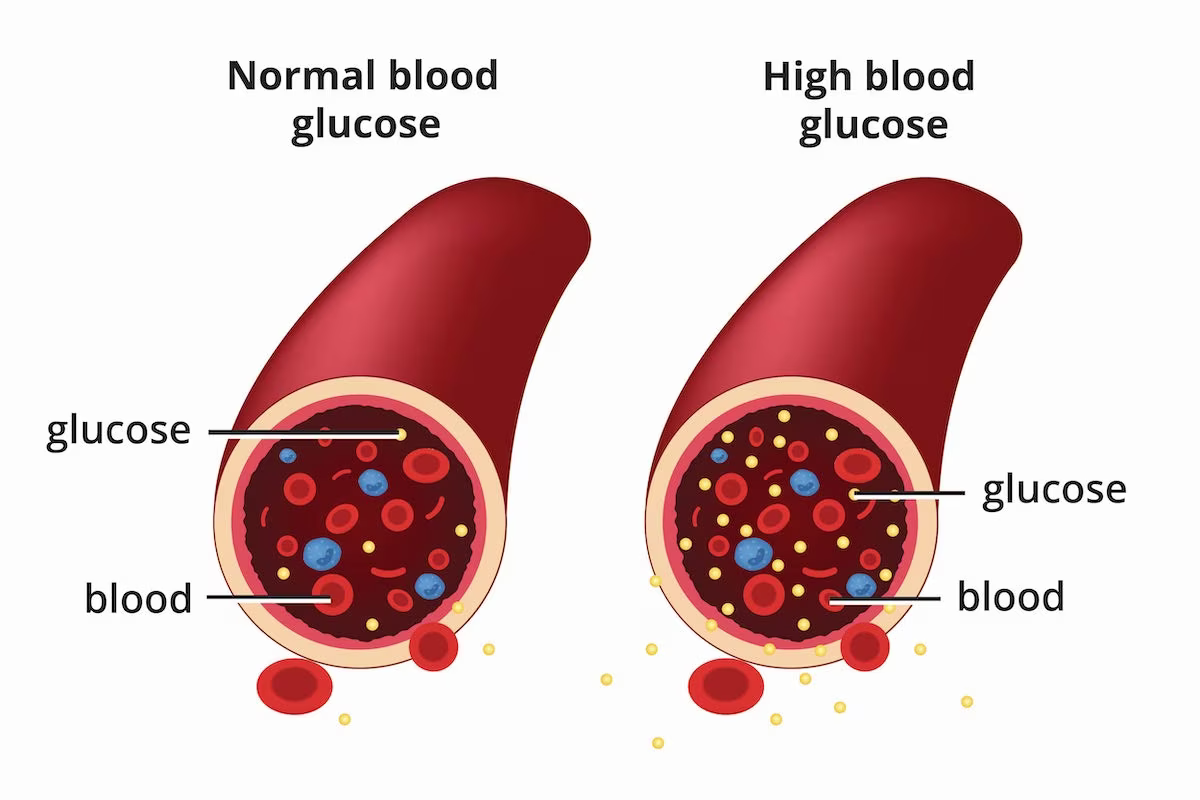
Diabetes is a disease that occurs when your blood glucose, also called blood sugar, is too high. Glucose is your body’s main source of energy Insulin is a hormone made by the pancreas that helps glucose get into your cells to be used for energy. If you have diabetes, your body doesn’t make enough—or any—insulin, or doesn’t use insulin properly. Glucose then stays in your blood and doesn’t reach your cells. Diabetes raises the risk for damage to the eyes, kidneys, nerves, and heart. Diabetes is also linked to some types of cancer. Taking steps to prevent or manage diabetes may lower your risk of developing diabetes health problems.

TYPES OF DIABETES
The most common types of diabetes are type 1, type 2, and gestational diabetes;
Type 1 diabetes
If you have type 1 diabetes, your body makes little or no insulin. Your immune system attacks and
destroys the cells in your pancreas that make insulin. Type 1 diabetes is usually diagnosed in children
and young adults, although it can appear at any age. People with type 1 diabetes need to take insulin
every day to stay alive.
Type 2 diabetes
If you have type 2 diabetes, the cells in your body don’t use insulin properly. The pancreas may be
making insulin but is not making enough insulin to keep your blood glucose level in the normal range.
Type 2 diabetes is the most common type of diabetes. You are more likely to develop type 2 diabetes if
you have risk factors, such as overweight or obesity, and a family history of the disease. You can
develop type 2 diabetes at any age, even during childhood.
You can help delay or prevent type 2 diabetes by knowing the risk factors and taking steps toward a
healthier lifestyle, such as losing weight or preventing weight gain.
Gestational diabetes
Gestational diabetes is a type of diabetes that develops during pregnancy. Most of the time, this type
of diabetes goes away after the baby is born. However, if you’ve had gestational diabetes, you have a
higher chance of developing type 2 diabetes later in life. Sometimes diabetes diagnosed during pregnancy
is type 2 diabetes.
Prediabetes
People with prediabetes have blood glucose levels that are higher than normal but not high enough to be
diagnosed with type 2 diabetes. If you have prediabetes, you have a higher risk of developing type 2
diabetes in the future. You also have a higher risk for heart disease than people with normal glucose
levels.
CAUSES OF DIABETES
What causes type 1 diabetes?
Type 1 diabetes occurs when your immune system, the body’s system for fighting infection, attacks and
destroys the insulin-producing beta cells of the pancreas. Scientists think type 1 diabetes is caused by
genes and environmental factors, such as viruses, that might trigger the disease. Studies such as
TrialNet External link are working to pinpoint causes of type 1 diabetes and possible ways to prevent or
slow the disease.
What causes type 2 diabetes?
Type 2 diabetes—the most common form of diabetes—is caused by several factors, including lifestyle
factors and genes.
Overweight, obesity, and physical inactivity
You are more likely to develop type 2 diabetes if you are not physically active and are overweight or
have obesity. Extra weight sometimes causes insulin resistance and is common in people with type 2
diabetes. The location of body fat also makes a difference. Extra belly fat is linked to insulin
resistance, type 2 diabetes, and heart and blood vessel disease. To see if your weight puts you at risk
for type 2 diabetes, check out these Body Mass Index (BMI) charts.
Insulin resistance
Type 2 diabetes usually begins with insulin resistance, a condition in which muscle, liver, and fat
cells do not use insulin well. As a result, your body needs more insulin to help glucose enter cells. At
first, the pancreas makes more insulin to keep up with the added demand. Over time, the pancreas can’t
make enough insulin, and blood glucose levels rise.
Genes and family history
As in type 1 diabetes, certain genes may make you more likely to develop type 2 diabetes. The disease
tends to run in families and occurs more often in these racial/ethnic groups:
African Americans
Alaska Natives
American Indians
Asian Americans
Hispanics/Latinos
Native Hawaiians
Pacific Islanders
Genes also can increase the risk of type 2 diabetes by increasing a person’s tendency to become
overweight or have obesity.
What causes gestational diabetes?
Scientists believe gestational diabetes, a type of diabetes that develops during pregnancy, is caused by
the hormonal changes of pregnancy along with genetic and lifestyle factors.
Insulin resistance
Hormones produced by the placenta NIH external link contribute to insulin resistance, which occurs in
all women during late pregnancy. Most pregnant women can produce enough insulin to overcome insulin
resistance, but some cannot. Gestational diabetes occurs when the pancreas can’t make enough insulin.
As with type 2 diabetes, extra weight is linked to gestational diabetes. Women who are overweight or
have obesity may already have insulin resistance when they become pregnant. Gaining too much weight
during pregnancy may also be a factor.
TESTING OF DIABETES
The only way you can find out if you or a loved one has diabetes is from blood tests that measure you
blood glucose (sugar) levels.
The different blood tests that could be used to diagnose diabetes are as follows:
Non fasting blood tests
(1) HbA1c
A hemoglobin A1C (HbA1C) test is a blood test that shows what your average blood sugar (glucose) level
was over the past two to three months. It’s a quick and simple test
where a small amount of blood is taken from a vein in your arm. This is different to a finger-prick
test, which is a snapshot of your blood sugar levels at that moment.
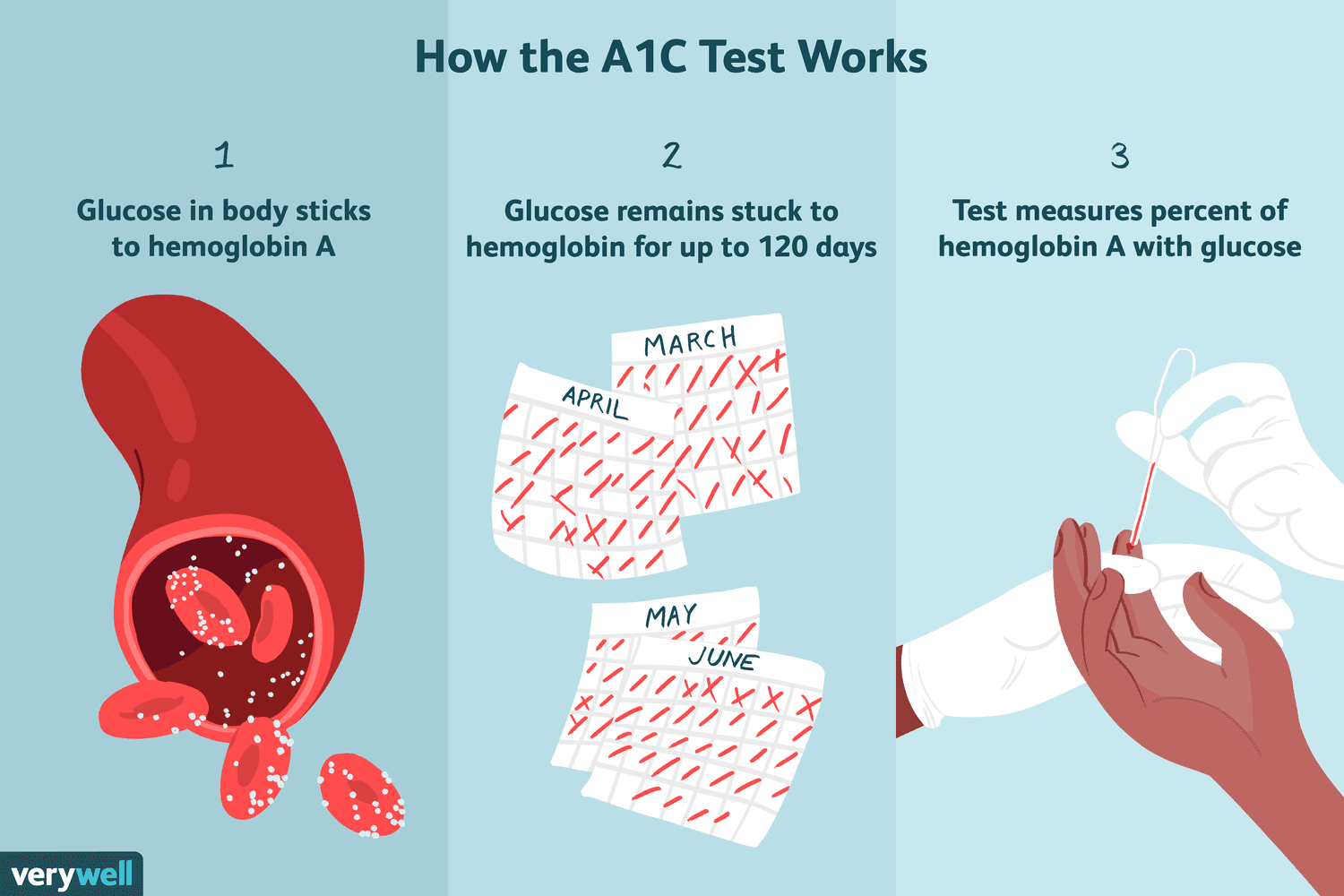
You have diabetes if your HbA1c level is 48mmol/mol or above.
You are at risk of developing type 2 diabetes (often known as prediabetes) if your HbA1c is between 42
and 48mmol/mol.
(2) Post Prandiol Test
The Post Prandial Blood Sugar Test is done two hours after you start eating your meals. It helps detect
prediabetes, type 1 diabetes, type 2 diabetes, gestational diabetes and other types of diabetes.
If
your
postprandial blood sugars are above 140-200 mg/dL, it indicates that you may have diabetes mellitus.
Normal Below 140 mg/dL Indicates normal blood sugar levels
Prediabetes 140 - 199 mg/dL Indicates a risk of developing diabetes- Prediabetes
Diabetes Above 200 mg/dL Indicates diabetes.
Other information about testing and diagnosis
Urine tests
A urine test for glucose on its own can’t diagnose diabetes. It will show your doctor if there is any
sugar in your urine, not how much or the possible cause.
Testing for diabetes at home
Home testing kits bought over the counter can’t diagnose diabetes. Neither can testing equipment used by
people with diabetes, like blood glucose meters. They will show only your blood sugar levels at the
moment you test.
Eye tests
An optician can’t diagnose diabetes. But during an eye test, they can spot eye damage that can affect
people with diabetes called diabetic retinopathy. They will then advise you to see your doctor to get
tested.
Type 2 diabetes screening by pharmacists
Some pharmacists offer short appointments where you can find out your risk of developing type 2
diabetes. You usually pay a fee for this service, which involves answering a series of questions.
A diabetes screening test does not diagnose you and is not completely accurate. Instead, it can be used
as a guide. Depending on the results from this screening, you or your loved one may be advised to seek
further medical help from your local GP. If you don’t appear to be at risk at the time of screening,
this doesn’t mean you aren’t still at risk of developing type 2 in the future. If you later find signs
of diabetes it’s worth being screened again, or being tested for diabetes.
Diabetes Diet, Eating, & Physical Activity
Nutrition and physical activity are important parts of a healthy lifestyle when you have diabetes. Along
with other benefits, following a healthy meal plan and being active can help you keep your blood glucose
level, also called blood sugar, in your target range. To manage your blood glucose, you need to balance
what you eat and drink with physical activity and diabetes medicine, if you take any. What you choose to
eat, how much you eat, and when you eat are all important in keeping your blood glucose level in the
range that your health care team recommends.
Becoming more active and making changes in what you eat and drink can seem challenging at first. You may
find it easier to start with small changes and get help from your family, friends, and health care team.
Eating well and being physically active most days of the week can help you
keep your blood glucose level, blood pressure, and cholesterol in your target ranges
lose weight or stay at a healthy weight
prevent or delay diabetes problems
feel good and have more energy
What foods can I eat if I have diabetes?
You may worry that having diabetes means going without foods you enjoy. The good news is that you can
still eat your favorite foods, but you might need to eat smaller portions or enjoy them less often. Your
health care team will help create a diabetes meal plan for you that meets your needs and likes.
The key to eating with diabetes is to eat a variety of healthy foods from all food groups, in the
amounts your meal plan outlines.
The food groups are :
vegetables
nonstarchy: includes broccoli, carrots, greens, peppers, and tomatoes
starchy: includes potatoes, corn, and green peas
fruits—includes oranges, melon, berries, apples, bananas, and grapes
grains
at least half of your grains for the day should be whole grains
includes wheat, rice, oats, cornmeal, barley, and quinoa
examples: bread, pasta, cereal, and tortillas
protein
lean meat
chicken or turkey without the skin
fish
eggs
nuts and peanuts
dried beans and certain peas, such as chickpeas and split peas
meat substitutes, such as tofu
dairy—nonfat or low fat
milk or lactose-free milk if you have lactose intolerance
yogurt
cheese.
Eat foods with heart-healthy fats, which mainly come from these foods:
oils that are liquid at room temperature, such as canola and olive oil
nuts and seeds
heart-healthy fish such as salmon, tuna, and mackerel
avocado
Use oils when cooking food instead of butter, cream, shortening, lard, or stick margarine.
Why should I be physically active if I have diabetes?
Physical activity is an important part of managing your blood glucose level and staying healthy. Being
active has many health benefits.
Physical activity
lowers blood glucose levels
lowers blood pressure
improves blood flow
burns extra calories so you can keep your weight down if needed
improves your mood
can prevent falls and improve memory in older adults
may help you sleep better
If you are overweight, combining physical activity with a reduced-calorie eating plan can lead to even
more benefits. In the Look AHEAD: Action for Health in Diabetes study,1 overweight adults with type 2
diabetes who ate less and moved more had greater long-term health benefits compared to those who didn’t
make these changes. These benefits included improved cholesterol levels, less sleep apnea, and being
able to move around more easily.
What physical activities should I do if I have diabetes?
Most kinds of physical activity can help you take care of your diabetes. Certain activities may be
unsafe for some people, such as those with low vision or nerve damage to their feet. Ask your health
care team what physical activities are safe for you. Many people choose walking with friends or family
members for their activity.
Add extra activity to your daily routine
If you have been inactive or you are trying a new activity, start slowly, with 5 to 10 minutes a day.
Then add a little more time each week. Increase daily activity by spending less time in front of a TV or
other screen.
Walk around while you talk on the phone or during TV commercials.
Do chores, such as work in the garden, rake leaves, clean the house, or wash the car.
Park at the far end of the shopping center parking lot and walk to the store.
Take the stairs instead of the elevator.
Light activities include
leg lifts or extensions
overhead arm stretches
desk chair swivels
torso twists
side lunges
walking in place
Do aerobic exercise,
Aerobic exercise is activity that makes your heart beat faster and makes you breathe harder. You should
aim for doing aerobic exercise for 30 minutes a day most days of the week. You do not have to do all the
activity at one time. You can split up these minutes into a few times throughout the day.
Do strength training to build muscle
Strength training is a light or moderate physical activity that builds muscle and helps keep your bones
healthy. Strength training is important for both men and women. When you have more muscle and less body
fat, you’ll burn more calories. Burning more calories can help you lose and keep off extra weight.
You can do strength training with hand weights, elastic bands, or weight machines. Try to do strength
training two to three times a week. Start with a light weight. Slowly increase the size of your weights
as your muscles become stronger.